Introduction
Caregiver burn out is defined as the physical, emotional, and mental exhaustion state accompanied by attitude change (McWilliam, et al., 2003). The attitude often changes from positive caring behaviors to negative care behaviors. Caregivers often feel guilty when they spend time away from the elderly person’s bestowed to their care. Burnout is often characterized with general fatigue, anxiety, and depression. To clearly understand burnout, it is important to differentiate it from depression or related cases. Often when burnout manifests itself as depression, the caregivers are tempted to resort to escapist behaviors which may include sexual irresponsibility, irresponsible drunkenness, drug abuse and other compulsive behaviors. The South Wales trends in relation to aged caregiver trends present several Scenarios worth studying.
This paper attempts to explain four possible future scenarios based on the trends and drivers surrounding the research topic. These drivers include increase of elderly people, nature of the aged care job, government funding, work conditions issues, organizational structure and ethical considerations. Based on these trends, four scenarios are developed. These are:
- High ethics versus structured work conditions
- Low ethics versus structured work conditions
- Low ethics versus unstructured work conditions
- High ethics versus unstructured work conditions
Ethics
Ethics relates to conduct code intended to guide individuals as they undertake their activities. Various persons have defined as a set of behavioral guidelines which focus on addressing the issue of morality within the context in which it is intended. In the workplace ethics is considered of fundamental importance if integrity is to be upheld. Other than workplace ethics, individual ethics contribute a lot to the general ethical concept. They determine the code in which an individual adheres in the quest to uphold their integrity and their surrounding. Generally, they enhance accountability and a feeling of responsibility towards life and hence the workplace.
In the context of caregivers, ethics involves consideration of the complex decision they have to make with regard to their clients. Ethical decision are further complicate by the obligations they owe to their patients and they are have to understand the decision that need to be made, who makes the decisions and most fundamental who is held responsible for decisions made with regard to their clients.
Sustained care-giving presents alter lifelong relationship into newer levels and reveal some complexities which had not earlier been anticipated. Care-givers beliefs and emotions are challenged forcing them to try and accustom to the newer realities that may at times be depressing and quite difficult for them ethical challenges often arise in the process of caring for the aged. Moral principles are therefore fundamental to the aged care workers. Their duty of care must fundamentally guide the decision they make with regard to the clients under their care. While ethics guide care-giving practices, they cannot wholly capture the challenges of sustained care-giving which is often characterized with plenty of unpredictable scenarios both from clients and the presented conditions of work.
Structured Work Conditions
Structured work conditions generally make reference to well planned work conditions. The caregivers under such an environment have well planned timed for caring for clients; they have set wages and relevant guidelines that facilitate their work activities. Some persons have referred to work conditions as work environments where rules and restrictions are prime to operations. These come in form of dress codes, strict operating hours and stringent behavioral guidelines among others.
Trends
Increase of elderly people
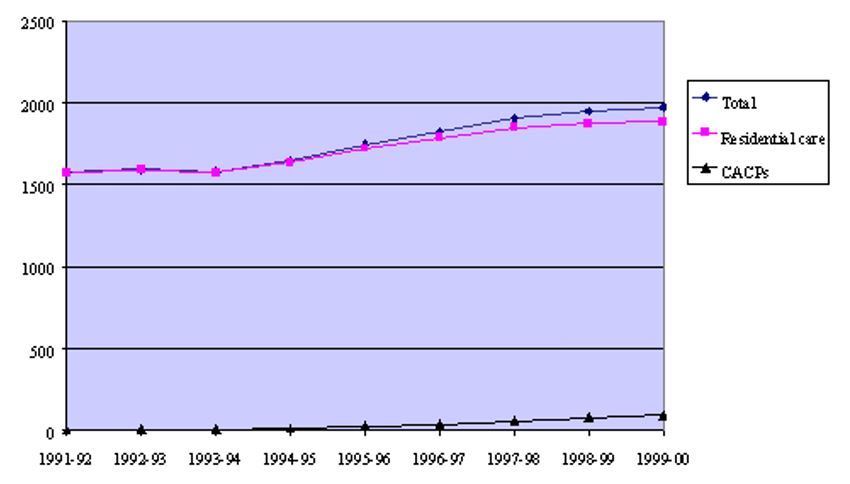
The ageing population in Australia is a product of declined fertility and increased life san/longevity as a result of better healthcare. It is estimated that currently the aged forms at least one percent of the whole population. These trends are exerted to rise to approximately 20% within the coming 40 years translating into an increased demand for aged care workers (Productivity Commission., 2008). The changing trends in aging population are best described with the tables below.
Table 1: Australian Aged Care Systems Profile (ABS Disability, Ageing and Carers Survey)
Table 2: Life Expectancy at Selected Ages (ABS Disability, Ageing and Carers Survey)
Various studies have found that caregivers for the aged were mostly females 87.5%, Our findings are similar to previous research findings in the study conducted by Joinson (2007) and Keidel (2008), who reported that the most caregivers are females. Most reports indicate that women make up about three quarters of all primary caregivers (Yancik, 1984: Van Staa, A. et al., 2006: Zerwekh, 2007: Joinson, 2007)
Studies have found that women provide more intensive care than do men. Male spousal caregivers are more likely than female spousal caregivers to obtain in-home services to aid in their responsibilities and sons and daughters tend to choose different solutions when care giving situations arise. For example, women are more likely to perform tasks such as cooking and cleaning, which often require more time or more frequent contact than do the tasks that males are more apt to perform, such as financial management and home repairs (Tennstedt, 1999).
Studies also show a negative relation between functional disability among the elderly and caregiver burden. Also our study revealed that there was negative relation between mental disability of elderly and caregiver burden. A summary of the caregiver’s demographic structure in South Wales is illustrated by the diagram below based on the findings from the center for the elderly statistics.
Table 3: New South Wales aged care Demographics
Most families prefer to take care of their aged ones at home while only a few prefer care centers and providers (Gold, 2001). Caregivers are therefore generally employed either on permanent or part-time basis in residential homes. This trend of co-residence is however attributed to reduced income levels where the families fear incurring more expenses on care home (Bickley, 2006). Co-residence with the elderly can therefore be termed as an act of necessity rather than desire. It is estimated that sharing hoses likelihood declines as the persons get more aged. Most caregivers operating in residential homes live around the residential areas and often there is no necessity for them to move in with the family.
Technology promises better ways that would assist caregivers dispense their responsibility in better ways. Nearly half of caregivers say some sort of technology has been used in the care of their recipient. The most prevalent technology used is an electronic organizer or calendar (24%) (Martin, 2002). Half as many say their care recipient has used an emergency response system like Lifeline (12%) or that the care recipient uses a device that sends information electronically to a doctor or a care manager (11%) (Productivity Commission, 2008). Nearly one in ten report use of a sensor that detects problems in the home, like when someone falls, wanders away, or leaves the stove on (9%), and 7% report use of a website or computer software to keep track of personal health records (Marino, 2009). Of six potential national policies or programs that could be offered to help caregivers, by far the most popular is a caregiver tax credit of $3,000. Half of caregivers rate it as the first or second most preferred policy. About three in ten prefer a voucher program where their care recipient could pay them minimum wage for at least some of their care giving hours (29% first or second choice), and a similar proportion prefer respite services (26%).
Nature of the job
Caring for the job is complex and rather demanding. The job requires lots of dedications and commitment other than treating it as an employment. Most persons often quit as a result of the conditions they are subjected in the line of job and inability to cope with the changing landscape of the job. Dealing with old persons is often cumbersome and requires a lot of patience and determination.
Various studies show that that the prevalence of burden among family caregivers for elderly was 37% (30% mild, 5. % moderate, 2 % severe) with mean burden score was 22. Many studies were conducted to determine the burden among caregivers of disabled elderly. Some studies are consistent with our results as that reported by Vachon, (2001) a study was conducted to target all disabled elderly and their principal caregivers residing in South Wales previously, found that burden among family caregivers for disabled elderly was 32.5 with mean burden score 28.7. Other study showed higher prevalence of burden as Karlikaya et al (2005) reported that 90% of the caregivers had some degree of burden.
Work conditions
Job attractiveness is always a dependent on several aspects. These include the working conditions presented to the employees and the remuneration/motivation they are accorded. While primarily aged care workers are motivated by the fact the elderly persons under their care need proper care and attention, other factors cannot be ignored. In a survey study of the reason for unattractiveness of care-giving job in austral, while respondent blatantly mentioned that the job was plagued with poor wages, inadequate staffing and lack of opportunities for educational advancement. Additional complaints cited that the work environments associated with caring for the aged were full of hostilities and increased pressure. Additionally, a research reported that facilitated with enhanced human resource practices and adequate staffing reflected more positive attitude of caregivers towards their job and likewise produced better physical and mental outcomes with regard to health. The complaints regarding working conditions are best illustrated by the recent complaints from workers about wages and work durations.
Government funding
The common wealth government is the chief funder and regulator of formal residential care in Australia. Its formal operations are constituted under the aged care act of 1997 and the aged care principles of 1997. Its main residential aged care strands include high care places, low care places and community aged care packages. As at 30 June 2006, there were 4000 occupied aged care homes in Australia providing a total of 152,162 places had been availed by the government. In addition, 18,149 community aged care packages were provided. Regarding funding, approximately 755 of available aged care funds are provided by the government. The government channels funds via the commonwealth’s health and aged care department. Additionally, veteran’s affairs for the aged, acts as a channel for funding of specific residential aged care initiatives.
An estimated $254 million were provided by the commonwealth government in 2007 as a capital component within its recurring subsidies to the facilities hosting the aged.
Scenarios development
The scenarios mentioned earlier are defined based on a number of conditions which affect the rate at which the aged care-workers may suffer from burnouts.
High ethics versus structured work conditions:
Work conditions with high ethics and structured conditions present an organized work environment where care is systematically administered. As mentioned earlier, the key factors that affect caregiver burnout rates include the conditions of works. Ethics is a fundamental aspect of human life. It begins with valuing fellow human beings and appropriate management of resources placed under ones care. Other than ethics, much stress is often placed on quality provision (Borys & Pope, 1989). Structured environments with high ethics, offer the ideal work environment t minimize caregiver burnout.
The structured care-giving environments offer professional environments that allow caregivers to operate professionally and within guided structures. Such environments acknowledge and respect regulations and guidelines that guide professional conduct. Researches have indicated that they are positive factors which affect the personality of caregivers including professional commitment, greater self-insight, more mature Social relationships, increased self-assurance and humility, reduced alienation and authoritarianism, and greater self-ideal congruence (Cherniss, 1980). However, professional caregivers are also faced with their own cup of challenges which make elimination of burnouts a mirage. While their professionalism and structured approach to work helps abet the same, clients presents a challenge to them. Deutch (1984) found that suicidal statements, expressions of anger toward the caregivers, severely depressed clients, apathy/lack of motivation, and client premature termination as the most significant sources of stress for professional caregivers. These results are almost identical to those Farber (1979) and Farber discovered in surveys of caregivers in eastern United States. Interestingly Coady, Kent, & Davis (1990) too presented interesting statistics revealing that stressful events form everyday life of caregivers for the aged. She reported that such stressful events occur hourly, if not daily, in the lives of full-time professional caregivers and make them a vulnerable target for the effects of stress. She further concluded that professional caregivers develop coping strategies as they get more seasoned in practice. Structured environments take into consideration all these factors and positively impact on the burnout rates keeping them at minimal. High ethics and structured environments provide ideal environments where caregivers are well informed of the coping strategies, their challenges are addressed through official channels, they are provide with adequate rest time and are offered preferably better pay packages.
Taking care of the aged calls for vast amount of resources usage, structured caregiver environments offer better paying opportunities for professional services offered by caregivers. Professional caregivers enjoy a position of power with their clients. Structured environments with high ethics facilitate their work by offering guidelines which ensure that their roles are helpful to their clients while at the same time avoiding over-involvement and under-involvement with the clients. Professional caregivers understand and work within this boundaries limiting their chances of suffering burnouts. Such boundaries included the listed below:
- Personal information sharing.
- Failure to see behavior as asymptomatic
- Giving clients nicknames or getting endeared to some at the expense of the others.
- Touch
- Professional Demeanor
- Accepting favors, gifts, tips from clients.
- Over-involvement
- Sexual Attraction/Relationships
- Keeping Secrets
The role of technology in care-giving remains largely important. Structured care-giving environments avail relevant and adequate knowledge to caregiver’s use of technology to their advantage. Caregiver’s use of technology begins with having the right knowledge and knowing exactly where to look. Medicine administration for instance can easily be aided with technology to ensure proper timing. Clinical documentation has generally been largely aided with the recent technological advancement and development of documentation software. Professional and structured work environments for caregivers largely apply the caregivers of technology in documentation.
Low ethics versus structured work conditions
Structure alone would be worthless if no structures are well outlined to facilitate the operations of the caregivers. Ethics are prime to the functioning of every organization. Non-ethical environments though structured subject the caregivers to increased stress rates as compared to high ethics structured environments (Brock, 1997). However, the structured environment offers guidelines that ensure that burnouts o not go to higher levels. Caregivers work often involves non-ordinary conscious states, expanded mediation, and psychic awareness. Other than, this strength is a necessity. Lack of coping capabilities makes the caregivers vulnerable to ethical misconduct which accelerates their burnout rate though not at very high rates.
Social life of caregivers is characterized with a number factors resulting from unethical working conditions presented to them. While caregivers often tempt to employ coping strategies in performing their work, often unethical working environments presents a lot to stressful situations. Among the social factors occurring as a result of unethical behaviors compromise the maximum levels of comfort that would have otherwise been offered by the structured environment in place. Structured environments, though offering better remuneration and guidelines, lack in mental environment necessary to fully cushion the caregivers from burnout. Other stress factors encountered by the caregivers within work environments, they are additionally vulnerable to cases of ethical misconduct which have a high likelihood of facing legal suits for medical malpractice. Such cases further stress the caregivers and increase the likelihoods of them suffering burnouts.
A study by Farber (1993) indicated that caregivers and psycho-caregivers behavior and attitudes are subject to the work experiences experienced. unethical work environments potential deteriorate the morale and urge of the worker to continue providing care. Farber further reported that salient changes resulting from unethical work environments of caregivers increased their psychological mindedness and ascription to their individual motivation and behavioral intentions. He further stated that quality acted as a “double-edged sword,” insofar as it enriched their lives with deeper meanings and assisted them in their careers but also negatively impacted their close personal relationships. In discussing his data, Farber quoted Henry (1966): “The career of the aged care professional, at least those in care practice, is a commitment to a lifestyle, as caregivers as an investment in a line of work.” This he mentioned calls for ethical behavior on the part of the caregivers and most importantly the environment in which they work.
Low ethics versus unstructured work conditions
Unstructured unprofessional work environments come with it’s of challenges. When accompanied with low ethics, the caregivers operate with less or no professionalism in addition to lack of adequate structural guidelines for the caregivers. Caregivers operating in this environment lack educational resources in the field and in addition lack any structured procedure of providing care to the elderly. These caregivers take lesser payments home and lack strategies to combat the effects of such. Most work on casual basis with no employment terms though in some circumstances, they are provided with permanent employment due to professional inadequacies. As already mentioned they receive low pay and hence lack the resources to take care of the heath related effects arising from the jobs they. Combined with lack of high ethics, they are more susceptible to burnout and research indicates that they are likely to suffer 100% burnout. Their quality of life and quality of service they produce is less.
Unprofessional and unstructured work environments are a leading cause of compassion fatigue amongst caregivers taking care of the aged. This arises when caregivers fail to create a balance between the time they give to their clients and the time they spend helping themselves. It is a product of caregivers focusing on the needs of others without engaging in self-sustaining healthcare practices which cover both financial, social life and technological aides. Important to mention too is that politics of the day determine how resources are allocated and in the end it’s the caregivers who work in unstructured and unprofessional environments who end up suffering insurmountable amounts of fatigue (Gentry, 2002). Compassion fatigue largely contributes to burnout of these groups of caregivers. Compassion fatigue originates from an internal place of depletion. Healthy caregivers fill themselves up and experience abundance. Those of caregivers with Compassion Fatigue deplete our emotional, physical, mental, and spiritual resources. Ultimately, caregivers are left with nothing to fortify and strengthen our resolve to be of service to others. Eventually, a wide range of destructive behaviors surface and create havoc in our lives. Due to a lack of understanding about what Compassion Fatigue is and the inability to skillfully manage the symptoms, caregivers often view themselves in negative ways, applying such labels as over-reactive, unprofessional, or possessing a savior complex. Others see caregivers as selfless, lacking in personal boundaries, and altruistic to a fault. With ill-fitting labels such as these, it isn’t common for caregivers working in unprofessional and unstructured environments to ask themselves: What is wrong with me? What don’t I feel happy? Why am I sad most of the time? Why doesn’t anyone understand me? Few have time to think that they may be suffering from compassion fatigue. Lack of technology worsens the situation as they lack relevant source of information. Information is important in freeing them from ignorance and lack of relevant knowledge to help them.
Compassion fatigue amongst caregivers in unprofessional environments is characterized with consistent thoughts of clients situation and condition, increased levels of negativity and anxiety, avoids of some client materials and occurrences which are painful, finding it difficult to separate work life from normal life, transference and countertransference with clients on some issues, spontaneous depression, disturbances resulting from own perception, increase level of self soothing and work ineffectiveness, and increased disdain for care-giving career. Additionally, the caregivers suffer a feeling of therapeutic impotence with regard to specific clients, diminished sense of usefulness and ego-functioning, loss of hope and increased occurrences of ethical violations. Despite indications that this type of fatigue is mainly transmitted from client to caregiver, the environment and the society are also widely believed to contribute to this transmission (Danieli, 1996).
Stress and burnout may therefore have significant consequences for both caregivers and patients in unstructured and unethical environments (Ramirez et al., 1998: 204). For example, a nurse’s strong emotional reaction to a patient’s suffering and diagnosis may result in her disengagement from or avoidance of the patient and his family or in chronic dissatisfaction with work. Clinicians, including nurses, may also fail to communicate necessary patient information to other providers, fail to attend to some details of care, or make contact with the patient more than is clinically necessary. Ultimately, burnout results in poor-quality care, including a failure to identify patient and family values and goals of care, which in turn leads to patient distrust.
Economic effects on caregivers is evidenced in instances where the caregivers functioning ability is impaired by the financial requirements of that particular task. With most institutional caregivers working away from home, financial factor is fundamental. In the state of California, it is projected that caregivers affected by financial difficulties have to juggle between their work duties, family life and care-giving responsibilities and approximately 28% have been forced to quit their responsibilities to care for their own family members (Figley, 1995). Generally, unethical and unstructured environments lead the pack when it comes to environments causing burnout amongst caregivers.
High ethics versus unstructured work conditions
Unstructured high ethics environments lack structures which facilitate communication between the involved stakeholders. Communication is often fundamental to success of any organization. Additionally, such environment applies limited technological use which has the potential of limiting care-giver burdens. Unstructured environments are long associated with stressful situations which impact on caregiver burnout rates. Though individual high ethics limits the levels to lower than unethical unstructured, the levels remain significantly high. For example, a nurse’s strong emotional reaction to a patient’s suffering and diagnosis may result in her disengagement from or avoidance of the patient and his family or in chronic dissatisfaction with work. Clinicians, including nurses, may also fail to communicate necessary patient information to other providers, fail to attend to some details of care, or make contact with the patient more than is clinically necessary. Ultimately, burnout results in poor-quality care, including a failure to identify patient and family values and goals of care, which in turn leads to patient distrust. Remuneration of caregivers is also a matter of concern in unstructured unethical environments. Lack of clear structures additionally, lead to poor time scheduling and have the potential of leaving the caregivers overburdened with work.
Caregivers for the old spend most of their time looking at their clients. They have little time to spend doing their own things and ultimately they need adequate finance to enable them pay for help with the other services. Having to deal with the long hours of caring for the aged and at the same time engaging in other exhaustive activities makes them tired and overstretched. The resulting stress is primarily the major cause of burnout for the professional caregivers.
Conclusion
“The findings indicate that workers in facilities with well-developed human resource management practices and adequate staffing levels report more positive attitudes towards their work and better physical and mental health outcomes. Individuals from these facilities also report that they are able to provide a higher quality of care for their residents.”
The need for clear ways aimed at keeping aged care workers to keep staff motivated and as comfortable as possible cannot be overstated. Aged care workers should be provided with adequate training on performance management practices crucial to their personal development and maturity. The importance of caregivers to increased age population in Australia cannot be overstated as statistics speak for themselves.
Care-giving is a diverse study area. The experiences involved range from those that are simple to manage to cases which demand a lot of tome and dedication from the caregivers. Fulfilling this roe without an overwhelmingly experience of physical, emotional and financial challenges remains a mirage. The caregivers are increasingly vulnerable to risks themselves including emotional stress, financial hardship and getting sick themselves. As already mentioned, in the coming years, the population of persons in need of assistance will continuously increase and will even renders the younger population option less when it comes to care-giving. With professional caregivers diminish in numbers, there exists likelihood that the caregivers then would basically lack necessary training and are even more likely to suffer burnouts. This is taking into consideration that the number of persons wiling to take up these roles contains to dwindle by the days. This essential means that in the future, professional caregivers will be older and will themselves be facing infirmity. The few existing caregivers then will have to handle more than one elderly person to meet the rising demand. Technology, however, comes as a relief solution. However, much needs to be done to secure the future of the elderly population living in south Wales and Australia in general.
It is therefore important that the following are done:
- Caregivers at risk of deteriorated health, financial insecurity and reduced quality of life, be identified early enough and appropriately assisted in maintenance of their individual well being while taking care of the aged.
- Programs that advocate for well being of caregivers and aimed at creating a difference in the caregivers lives be initiated to ensure that they are health and capable of continuing to offer this vital service.
- Use of technology, be incorporated into care-giving practices and information dissemination to the caregivers.
- The aforementioned program, be availed to all caregivers regardless of age and financial position.
- Educate and encourage families and Caregivers on the best practices that facilitate proactive planning for their aging ones and hence reduce dependence years.
High level of professionalism and integrity is important for caregivers taking care of the aged. This principle addresses a wide variety of issues including criteria for revocation of clinical membership in caregiver association if the caregiver is convicted of a felony or any other behavior related to his or her functioning in the capacity of a marriage and family therapist (e.g., misdemeanor, incompetent practicing while impaired, disciplinary action by another professional organization, and failure to comply. This principle also includes guidelines for behaviors such as seeking professional assistance for personal problems; dedication to high standards as teachers, researchers, and supervisors; maintaining current knowledge of developments in the field; prohibition of sexual harassment; restricting therapeutic practice to areas of competency; maintenance of integrity in reporting research findings; and a prescription to exercise special care when making public professional recommendations and opinions.
Additionally, Caregivers need to uphold confidentiality of information regarding the aged laced under their care. They must protect the information and make sure that it is used for no purposes other than assisting the client. This principle provides specific guidelines for the maintenance and release of client information by marriage and family caregivers. Caregivers for the aged advance the welfare of families and individuals. They need to exercise high ethics and respect to the persons placed under their care and reasonably act for the advancement of their welfare. This principle provides sanctions against discrimination, exploitation, and dual relationships that might impair judgment or involve sexual engagement, self-interest, continuing a therapist-client relationship when it is not helpful, and abandonment of clients (Gibson, McGrath & Reid, 1989).
References
Bickley, J. B., 2006. Care for the caregiver: the art of self-care. Semin Perioper Nurs, 7(2), p 114-21.
Borys, D., & Pope, K., 1989. Dual relationships between Caregiver and client: A national study of psychologists, psychiatrists, and social workers. Professional Psychology. Research & Practice, 20(5), p 283-293.
Brock, G.W., 1997. Reducing vulnerability to ethics code violations: An at-risk test for marriage and family therapists. Journal of Marriage and Family Therapy, 23 (1), p 87-89.
Cherniss, C., 1980. Professional burnout in human service organizations. New York: Praeger.
Coady, C.A., Kent, V.D., & Davis, P.W., 1990. Burnout among social workers working with patients with cystic fibrosis. Health and Social Work, 15(2), p 116-124.
Danieli, Y., 1996. Who takes care of the caregiver? In R.J. Apfel & B. Simon
Farber, B. A., & Heifetz, L. J., 1982. The process and dimensions of burnout in psychotherapists. Professional Psychology, 13, p 293-301.
Farber, B., (1983). The effects of psychotherapeutic practice upon psychotherapists. Psychotherapy. Theory, Research and Practice, 20(2), p 174 –182.
Farber, S. J. et al., 2007. Issues in end-of-life care: patient, caregiver, and clinician perceptions. J Palliat Med, 6(1), p 19-31.
Figley, C. R., 1995. Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. New York: Bruner/Mazel.
Figley, C.R., 2002. In C. Figley (Ed.), Treating compassion fatigue. New York : Gentry, J.E., 2002. Compassion fatigue: The crucible of transformation. The Journal of Trauma Practice, 1(3-4), p 37-61.
Gibson, F., McGrath, A., & Reid, N., 1989. Occupational stress in social work. British Journal of Social Work, 19, p 1-16.
Gold, J., 2001. Thornton L. Simple strategies for managing stress. RN, 64(12):65.
Joinson, C., (2007). Coping with compassion fatigue. Nursing, 22(4), p 116, 118-9, 120.
Keidel, G. C., 2008. Burnout and compassion fatigue among hospice caregivers. Am J Hosp Palliat Care, 19 (3), p 200-5.
Marino, P. A., 2009. The effects of cumulative grief in the nurse. J Intraven Nurs, 21(2), p 101-4.
Martin, B., 2002. Promoting balance between personal health and professional responsibility. Chart, 99(5), p 4-5.
McWilliam, C. L, et al., 2003. The challenging experience of palliative care support team nursing. Oncol Nurs Foru, 20 (5), p 779-85.
Productivity Commission., 2008. Trends in Aged Care Services: some implications, Commission Research Paper, Canberra.
Ramirez, A. et al., 1998. ABC of palliative care: The Carers. BMJ, 316 (7126), p 208-11.
Shanafelt, T. D. et al., 2006. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med, 136(5), p 358-67.
Vachon, M. L., 2001. The nurse’s role: the world of palliative care nursing. In: Ferrell B, Coyle N, editors. The textbook of palliative nursing. New York: Oxford,. p. 647-62.
Vachon, M. L., 2007. Reflections of the history of occupational stress in hospice/palliative care. Hospice Journal, 14(3), p 229-46.
Vachon, M. L., 2008. Caring for the caregiver in oncology and palliative care. Semin Oncol Nurs, 14(2). p 152-7.
Vachon, M. L., 2009. Staff stress in hospice/palliative care: a review. Palliat Med, 9 (2), p. 91-122.
Van Staa, A. et al., 2006. Caring for caregivers: experiences and evaluation of interventions for a palliative care team. Patient Educ and Counts, 4(1), p 93-105.
Wright, S., 2000. Look for the healer inside yourself. Nurs Stand, 15(6), p 22.
Yancik, R., 1984. Coping with hospice work stress. J Psychsoc Oncology, 2(2), p 19-35.
Zerwekh, J., 2007.Transcending life: the practice wisdom of nursing hospice experts. Am J Hosp Palliat Care, 10(5), p 26-31.